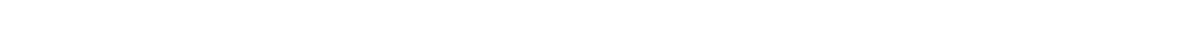
TMS vs. medication comes down to treatment approach and side effects. TMS uses targeted magnetic pulses to stimulate brain areas linked to mood without systemic side effects. Medication works by altering brain chemistry but can cause side effects like weight changes or fatigue. TMS is often chosen when medications are ineffective or not well tolerated.
What Is Depression and Why Does It Need Treatment?
Depression is more than just feeling sad. It's a real medical condition that affects how you think, feel, and handle daily tasks. People with depression often feel empty, hopeless, or unable to enjoy things they once loved.
Depression happens when parts of your brain that control mood don't work right. This can be caused by chemical imbalances, stress, genes, or life events. Without treatment, depression can get worse and affect your work, relationships, and physical health. That's why getting professional help through psychiatric care is so important.
The good news? Depression is treatable. Most people feel better with the right help whether that's medication, therapy, TMS, or a combination of treatments.
How Antidepressant Medications Work
Antidepressant medications work by changing the levels of certain chemicals in your brain. These chemicals, called neurotransmitters, help brain cells talk to each other. When they're balanced, your mood improves. Different types of antidepressants target different brain chemicals, which is why some work better for certain people than others. Understanding how these medications function can help you make informed decisions about your treatment.
Types of Antidepressant Medications
There are several types of antidepressants, and doctors usually start with the ones that have fewer side effects.
SSRIs (Selective Serotonin Reuptake Inhibitors) are the most common type. They increase serotonin, a brain chemical that affects mood. Examples include Prozac, Zoloft, and Lexapro. Doctors often prescribe SSRIs first because they generally cause fewer problems than older drugs.
SNRIs (Serotonin and Norepinephrine Reuptake Inhibitors) work on two brain chemicals: serotonin and norepinephrine. Examples include Cymbalta and Effexor. SNRIs might help if SSRIs don't work well enough.
Tricyclic Antidepressants (TCAs) are older medications that affect multiple brain chemicals. They work well but often cause more side effects, so doctors save them for cases where newer drugs haven't helped.
There are also atypical antidepressants like Wellbutrin and MAOIs, which work differently from the other groups. Doctors prescribe these when standard options don't provide relief.
How Long Do Medications Take to Work?
Antidepressants don't work right away. Most people need to wait 3 to 6 weeks before they notice real improvement. Some people feel a bit better in the first week or two, but full benefits take time.
Your doctor might adjust your dose or switch medications if the first one doesn't help enough. Finding the right medication often means trying different options.
Common Side Effects of Antidepressant Medications
All medications can cause side effects, and antidepressants are no exception. The good news is that many side effects are mild and go away after a few weeks. However, understanding what to expect can help you prepare and communicate better with your doctor. Some side effects are more common than others, and knowing the difference between typical reactions and serious concerns is important for your safety.
Physical Side Effects
Common physical side effects include upset stomach or nausea, dry mouth, headaches, dizziness, feeling tired or drowsy, trouble sleeping, and changes in appetite and weight. Some people also experience sexual problems, like low interest in sex or difficulty reaching orgasm. These side effects can be frustrating and may lead people to stop taking their medication.
Serious Side Effects (Less Common)
While rare, some serious side effects can happen. These include increased thoughts of suicide (especially in young people under 25), serotonin syndrome (when serotonin levels get too high), heart rhythm problems, and bleeding problems when combined with blood thinners. If you experience any unusual symptoms, contact your doctor right away.
Stopping Medications Can Be Hard
You can't just quit antidepressants suddenly. Stopping too fast can cause withdrawal symptoms like dizziness, nausea, anxiety, and feeling like you have the flu. Your doctor will help you slowly reduce your dose when it's time to stop.
What Is TMS Therapy?
Transcranial Magnetic Stimulation (TMS) is a newer way to treat depression without using drugs. The FDA approved it in 2008 for adults with depression who haven't responded to medication. Unlike traditional treatments that affect your whole body, TMS targets specific areas of your brain using magnetic pulses. This focused approach means fewer side effects and better results for many people. Let's explore how this innovative treatment works and what makes it different from medication.
How TMS Works
TMS uses magnetic pulses to wake up the part of your brain that controls mood. Think of it like a gentle wake-up call for brain cells that have become quiet because of depression.
During treatment, you sit in a chair while a device placed near your head sends magnetic pulses to a specific brain area called the dorsolateral prefrontal cortex. This region plays a big role in mood, emotions, and decision-making.
The magnetic pulses don't hurt, and you stay awake the whole time. Each session lasts about 20 to 40 minutes, and you can go back to your normal day right after.
TMS Treatment Schedule
A typical TMS course involves 20 to 30 sessions, five days a week, over four to six weeks. Most people start feeling better after four to six weeks of treatment. Some notice improvements earlier, while others need the full course.
Is TMS Safe?
Yes, TMS is very safe. The most common side effect is a mild headache or scalp discomfort during treatment, which usually goes away within the first week. Unlike electroconvulsive therapy (ECT), TMS doesn't cause memory loss or require anesthesia.
The most serious side effect is seizures, but this is extremely rare happening in about 1 in 200 patients. TMS providers are trained to handle this if it occurs.
TMS Side Effects vs. Medication Side Effects

When comparing TMS and medication side effects, TMS has a clear advantage. Side effects are one of the main reasons people stop taking antidepressants or look for alternative treatments. The difference in how these treatments affect your body is significant and worth understanding. While both options have some side effects, the severity and duration vary greatly between the two approaches.
TMS Side Effects
The most common TMS side effect is a mild headache, followed by scalp discomfort at the treatment site. Some people experience lightheadedness or facial twitching during pulses, though this is rare. The most serious side effect is seizure, but this is extremely rare happening in about one in 200 patients.
Most TMS side effects are temporary and mild. They usually fade within the first week of treatment.
Medication Side Effects (More Common and Longer-Lasting)
Antidepressants affect your whole body, not just your brain. This means they can cause side effects throughout your system, including stomach problems, sexual dysfunction, weight changes, sleep issues, and withdrawal symptoms when stopping.
Many people stop taking antidepressants because of these side effects. In fact, studies show that side effects get more likely as you add more medications.
Success Rates: Does TMS or Medication Work Better?
Let's look at the numbers to see which treatment helps more people. Success rates are one of the most important factors when choosing a depression treatment. While both options can be effective, the statistics show some clear differences. Understanding these numbers can help you set realistic expectations and make an informed choice about your care.
Medication Success Rates
Research shows that antidepressants help about 30 to 40% of people achieve significant improvement or remission. The STAR*D study, one of the largest antidepressant research projects, found that only about 33% of patients achieved remission with their first medication.
Each time you try a new medication after one fails, your chances of success go down. By the fourth medication, success rates drop even more.
TMS Success Rates
TMS shows higher success rates, especially for people who haven't responded to medications. The response rate (noticeable improvement) ranges from 50 to 75%, while the remission rate (symptoms gone completely) ranges from 30 to 50%.
In real-world studies with over 1,000 patients, about 75% experienced a clinical response to TMS, and nearly half achieved full remission.
TMS Works Even After Medications Fail
Here's what makes TMS special: it works even for people who've already tried multiple antidepressants without success. Studies show that around 30% of medication-resistant patients still respond to TMS therapy.
Who Is a Good Candidate for TMS?
TMS isn't for everyone, but it works well for many people with depression. Knowing whether you're a good candidate can save you time and help you focus on the right treatment path. There are specific criteria that insurance companies and doctors use to determine if TMS is appropriate for you. Let's break down who benefits most from this treatment and who should look at other options.
Good Candidates for TMS
You might be a good candidate if you have been diagnosed with major depressive disorder, haven't gotten enough relief from at least two different antidepressants, can't tolerate medication side effects, want a drug-free treatment option, or are 15 years or older. The FDA recently approved TMS for adolescents aged 15 to 21 with depression.
Most insurance companies require that you've tried medications first before they'll cover TMS. This makes sense because doctors want to start with less intensive treatments.
Who Should Not Use TMS
TMS isn't safe for everyone. You can't have TMS if you have metal implants in your head (except dental fillings), have a pacemaker or other implanted medical device, have a history of seizures or epilepsy, or are pregnant (more research is needed).
Your doctor will do a thorough evaluation to make sure TMS is safe for you.
Can You Combine TMS and Medication?
Yes! Many people use TMS and medication together, and research shows this combination can work even better than either treatment alone. You don't have to think of these as competing options. In fact, combining treatments is a common and effective strategy that many psychiatrists recommend. This approach can give you the benefits of both while potentially reducing the doses needed for each.
A 2019 study found that combining TMS with antidepressants led to higher remission rates than medication alone. TMS can boost the effects of your current medication or help you reduce your dose over time.
Your psychiatrist will create a treatment plan that's right for you. Some people eventually stop medications after successful TMS treatment, while others continue with a lower dose.
How Much Does Each Treatment Cost?
Cost is a big factor when choosing between TMS and medication. Healthcare expenses can add up quickly, especially when you're dealing with a long-term condition like depression. Understanding the financial commitment for each option helps you plan better and explore insurance coverage. Let's break down what you can expect to pay for both treatments and how insurance might help.
Medication Costs
Monthly antidepressant costs vary widely. Generic SSRIs typically cost $10 to $30 per month with insurance, while brand-name medications can run $100 to $500 per month. Without insurance, you might pay $30 to $200 or more per month.
Over time, these costs add up. If you take antidepressants for years, you'll spend thousands of dollars. Plus, there are costs for doctor visits, lab work, and trying different medications.
TMS Costs
A full course of TMS therapy typically costs $6,000 to $15,000 for the complete treatment, with an average of $300 to $500 per session. Most courses include 20 to 30 sessions total.
This might sound expensive, but remember that TMS offers lasting results. Most people don't need ongoing treatment after the initial course.
Insurance Coverage
The good news: most insurance companies now cover TMS for treatment-resistant depression. Major insurers including Medicare, Aetna, Cigna, Blue Cross Blue Shield, and UnitedHealthcare cover TMS when you meet certain requirements.
To get insurance coverage for TMS, you typically need a diagnosis of major depressive disorder, documentation that you've tried at least two antidepressants, proof that medications haven't worked or you can't tolerate them, and pre-authorization from your insurance company.
Medicare covers up to 80% of TMS costs, with patients paying the remaining 20% through coinsurance or secondary coverage.
Treatment Timeline: How Long Each Takes
Time is important when you're suffering from depression. Let's compare how long each treatment takes to work. When you're dealing with depression, every day matters. Knowing what timeline to expect helps you stay patient with your treatment and understand when you should see results. The speed at which treatments work can also affect your quality of life and ability to function in your daily activities.
Medication Timeline
During weeks one to two, you might notice some small changes, but most side effects happen now. Real improvements begin to show in weeks three to six. Full benefits become clear around weeks six to eight. After that, you need to keep taking medication daily, possibly for years.
If the first medication doesn't work, you'll need to wait another six to eight weeks to try a new one. This trial-and-error process can take months.
TMS Timeline
In week one, treatment starts and side effects are usually mild. Some people begin noticing improvements in weeks two to four. Most people see significant benefits in weeks four to six. After treatment ends, effects last for months, with an average of over a year.
TMS works faster for many people. Plus, once you complete treatment, you don't need daily sessions. Some people come back for maintenance sessions if symptoms return, but many stay better for a year or longer.
Long-Term Results and Maintenance
What happens after your initial treatment ends? Understanding the long-term picture is just as important as knowing how treatments work in the short term. Some treatments require ongoing maintenance, while others offer more lasting relief. The difference in long-term commitment between medication and TMS is one of the most significant factors to consider when making your choice.
Medication: Ongoing Treatment Required
Antidepressants require daily use to maintain their benefits. If you stop taking them, your depression symptoms often come back. Many people take antidepressants for years or even a lifetime.
There's also the risk of tolerance when your medication stops working as well over time. This means you might need dose increases or medication changes.
TMS: Lasting Relief
TMS offers more lasting relief. Research shows that most people feel better for many months after treatment, with the average response lasting over a year. About two-thirds of people who achieve remission stay symptom-free for 12 months. Maintenance sessions can extend benefits further.
If symptoms return, you can have another round of TMS. Studies show that 78% of people respond well to TMS again if they need retreatment.
Which Treatment Should You Choose?

Choosing between TMS and medication depends on several factors. There's no one-size-fits-all answer to this question. Your personal situation, medical history, treatment goals, and lifestyle all play a role in determining which option is best for you. Here are some guidelines to help you think through your decision, but remember that your doctor's input is essential in making the final choice.
Consider Medication First If You:
Consider medication first if you haven't tried antidepressants yet, have mild to moderate depression, prefer a lower-cost initial treatment, can tolerate side effects, or want convenience (just taking a daily pill).
Consider TMS If You:
Consider TMS if you have tried two or more antidepressants without success, can't handle medication side effects, want a drug-free option, have treatment-resistant depression, prefer a treatment with lasting results, or can commit to daily sessions for several weeks.
Both Treatments Work Together
You don't have to choose just one. Many people find that combining TMS with medication gives them the best results. Your psychiatrist can help you decide if this approach is right for you. Some patients benefit from medication management alongside TMS therapy to optimize their treatment outcomes.
Other Depression Treatments to Consider
TMS and medication aren't your only options. Here are other treatments that might help. Depression treatment has evolved significantly over the years, and today you have access to multiple evidence-based approaches. While TMS and medication are two primary options, combining them with other treatments or exploring alternatives might give you even better results. Let's look at what else is available.
Psychotherapy
Talk therapy, especially Cognitive Behavioral Therapy (CBT), helps many people with depression. Research shows CBT can be as effective as medication for some people, with response rates of 61 to 87%. Therapy teaches you tools to manage negative thoughts and behaviors. Many patients find that combining psychotherapy with other treatments provides the most comprehensive approach to recovery.
Combining therapy with medication or TMS often gives the best results.
Lifestyle Changes
Don't underestimate the power of regular exercise, good sleep habits, healthy eating, stress management, and social connections. These changes won't cure severe depression by themselves, but they support your treatment and improve your overall well-being.
Other Brain Stimulation Options
For severe, treatment-resistant depression, other options include electroconvulsive therapy (ECT), vagus nerve stimulation, and ketamine or Spravato treatment. Your doctor can discuss these if standard treatments haven't helped.
Real Patient Experiences
Understanding how treatments affect real people helps put the numbers in perspective. Statistics and success rates tell part of the story, but hearing about actual patient experiences can help you understand what to expect on a personal level. While everyone's journey is different, there are common themes that emerge when people share their experiences with medication and TMS.
Medication Experiences
Many people find relief with antidepressants. They appreciate the convenience of taking a daily pill and feel grateful when it works. However, others struggle with side effects like weight gain, sexual problems, or feeling emotionally numb.
Some patients describe trying multiple medications over months or years, dealing with different side effects each time. The trial-and-error process can be exhausting.
TMS Experiences
People who choose TMS often describe it as a last resort after medications failed. Many report being surprised by how painless and easy the treatment is. They like that they can drive themselves to appointments and go straight back to work or home.
Some notice their mood lifting gradually over weeks, while others have sudden "aha" moments where they realize they feel like themselves again. The lack of side effects is often mentioned as a huge relief.
Getting Started with TMS Therapy
If you're interested in TMS, here's what to expect. The process of starting TMS therapy is straightforward, but it involves several important steps. Knowing what happens at each stage can help reduce any anxiety you might feel about trying a new treatment. From your first evaluation to your daily sessions, here's a complete walkthrough of the TMS journey.
Step 1: Evaluation
You'll meet with a psychiatrist who will review your medical history, confirm your depression diagnosis, check which medications you've tried, make sure TMS is safe for you, and discuss your treatment goals.
Step 2: Insurance Approval
Your TMS provider will work with your insurance company to get pre-authorization. They'll submit documentation showing you meet the requirements for coverage.
Step 3: Brain Mapping
Before your first real treatment, your TMS technician will find the right spot on your head, adjust the magnetic pulse strength, and make sure the settings are comfortable for you.
This process is called motor threshold testing and helps personalize your treatment.
Step 4: Treatment Sessions
You'll come in five days a week for four to six weeks. Each visit lasts about 20 to 40 minutes. You can read, listen to music, or just relax during treatment.
Most people fit TMS sessions into their lunch break or before/after work.
Making Your Decision
Choosing between TMS and medication is a personal decision that should involve your doctor. Here are some questions to ask yourself. Making an informed choice requires honest self-reflection and open communication with your healthcare team. These questions are designed to help you think through the important factors that should influence your decision. Take your time with this process there's no rush, and the right answer will become clearer as you gather information.
Have I given medications a fair try (at least two different types for six to eight weeks each)? How much do side effects affect my daily life? Can I commit to daily TMS sessions for several weeks? Does my insurance cover TMS? Am I looking for a quick-start option (medication) or lasting results (TMS)? Would I benefit from trying both together?
Remember that depression treatment isn't one-size-fits-all. What works for someone else might not work for you, and that's okay. The most important thing is finding a treatment that helps you feel better.
Final Thoughts
Both TMS therapy and antidepressant medications can effectively treat depression, but they work in very different ways. Medications change brain chemistry throughout your body and require daily use. TMS targets specific brain areas with magnetic pulses and offers longer-lasting relief without the systemic side effects.
For many people, medication is the right first step it's convenient, covered by insurance, and helps millions of people every year. But if medications haven't worked for you, or if side effects make them unbearable, TMS offers real hope.
The numbers speak for themselves: TMS helps 50 to 75% of people who haven't responded to medications, with lasting results that often extend beyond a year. And with most major insurance companies now covering TMS, it's more accessible than ever.
If you're struggling with depression and haven't found relief, don't give up. Talk to your doctor about whether TMS might be right for you. At South Florida Medical Group, we offer comprehensive evaluations and treatment options to help you find the approach that works for you.
Your path to feeling better starts with understanding your options. Whether you choose medication, TMS, or a combination of treatments, know that effective help is available. You deserve to feel like yourself again.
Ready to take the next step? Contact our team today to schedule your mental health evaluation and explore your treatment options. We offer specialized NeuroStar TMS therapy for patients who haven't responded to traditional treatments. We're here to help you find relief and reclaim your life.
.png)
.png)
.png)



.png)
.png)
.png)

.png)

.png)