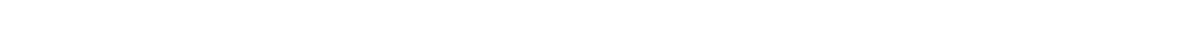
Family practice physicians provide broad medical care, but they have clear limits. They cannot perform major surgeries, prescribe controlled substances without medical need, or treat complex conditions outside their training, like advanced cancer or heart surgery. They also cannot practice independently in specialties like psychiatry or obstetrics without certification. Their focus stays on primary care, prevention, and referrals to specialists when needed.
Can Family Doctors Treat Their Own Family Members?
Family physicians cannot treat immediate family members except during emergencies or for minor health issues. The American Medical Association Code of Medical Ethics prohibits physicians from providing regular care to spouses, children, parents, or siblings.
Personal relationships compromise professional judgment. Doctors may avoid asking sensitive questions or performing intimate parts of the physical examination on family members. Patients may withhold important health information from physician relatives. Family members often hesitate to decline treatment recommendations or request different providers.
The American Board of Family Medicine lists self-treatment restrictions as grounds for licensure violations. State medical boards impose practice limitations on physicians who treat family members inappropriately. Physicians with licensure restrictions cannot maintain full board certification, affecting hospital privileges and insurance panel participation.
Emergency exceptions apply when no other qualified physician can provide care. Rural physicians in isolated locations may treat family temporarily until another doctor becomes available. Short-term minor problems like colds or small wounds fall within acceptable boundaries.
Physicians who treat family members must document all care provided. Documentation must transfer to the patient's primary care physician immediately. Physicians cannot prescribe controlled substances to immediate family except during true medical emergencies.
A gastroenterologist prescribed pain medication to his wife without accessing her psychiatric records. He failed to recognize signs of addiction, leading to overdose and hospitalization. The state medical board suspended his license and required supervised practice before reinstatement.
What Prescribing Restrictions Do Family Doctors Face?
Family physicians cannot prescribe controlled substances without proper Drug Enforcement Administration registration and mandatory training. The DEA requires all prescribers to complete eight hours of substance use disorder education before registration or renewal.
Federal law restricts Schedule II medication prescribing through telemedicine. Physicians need special telemedicine registration to prescribe stimulants, opioids, and other highly addictive medications without prior in-person evaluation. The Ryan Haight Act established these requirements to prevent online prescription drug abuse.
State prescription drug monitoring programs track controlled substance prescriptions. Physicians must check these databases before prescribing Schedule II-V medications. Most states now require checks within 24 hours of prescribing, creating workflow challenges for busy practices.
Self-prescribing controlled substances violates professional ethics except during acute emergencies. State medical boards sanction physicians who self-prescribe narcotics, viewing the practice as evidence of substance use disorder requiring treatment and monitoring.
Geographic restrictions complicate prescribing authority. Physicians can only prescribe to patients located in states where they hold active medical licenses. Insurance company formularies specify which drugs receive coverage at various cost-sharing tiers. Physicians must prescribe formulary medications or complete prior authorization requests.
Quantity limitations prevent stockpiling and diversion. Pharmacies restrict controlled substance fills to 30-day supplies in most cases. Some states limit initial opioid prescriptions to seven days for acute pain conditions.
What Surgical Procedures Can Family Doctors Not Perform?
Family physicians cannot perform major surgical operations, complex invasive procedures, or surgeries requiring specialized training. Medical training limitations prevent family doctors from conducting neurosurgery, cardiac surgery, organ transplants, or orthopedic joint replacements.
Family medicine residency programs teach minor office procedures. Doctors learn to remove skin lesions, drain abscesses, suture simple lacerations, perform joint injections, and treat ingrown toenails. Residency training typically includes fewer than 100 hours of procedural education compared to thousands of hours for surgical residents.
State laws prohibit family physicians from performing advanced surgical procedures without additional certification. Florida regulations restrict laparoscopic surgery to physicians with board certification in minimally invasive surgery. Hospital credentialing committees review each physician's surgical training and experience based on residency documentation, procedure logs, and continuing education records.
Malpractice insurance policies exclude coverage for procedures outside the physician's training. Insurance companies deny claims when doctors attempt surgeries beyond their scope of practice. These lawsuits often result in large settlements because performing procedures without proper training constitutes negligence.
The procedural scope varies dramatically between practice settings. Rural family physicians often maintain broader procedural skills due to limited specialist access. Urban family doctors focus on office-based preventive care and chronic disease management.
How Does Scope of Practice Limit Family Physicians?
Every medical specialty has a defined scope of practice that legally restricts the services physicians can provide. State medical practice acts outline specific procedures, treatments, and patient populations each specialty can serve.
Research shows individual family physician scope of practice decreases over time despite broader field capabilities. Doctors in urban areas with abundant specialists perform fewer procedures than rural practitioners. Insurance reimbursement policies, malpractice concerns, and patient expectations shape practice patterns.
Geographic location significantly affects scope limitations. Rural family physicians often provide obstetrics care, hospital medicine, emergency medicine services, and minor surgery due to specialist shortages. Urban family doctors focus primarily on outpatient preventive care and chronic disease management including hypertension control and diabetes monitoring.
Hospital bylaws restrict physician practice within healthcare facilities. State licensing boards sanction physicians who practice outside their scope. Penalties include mandatory practice limitations, required supervision, license suspension, or complete revocation.
Telemedicine expands geographic reach while maintaining scope limitations. Family physicians can provide telehealth services across state lines with proper licensing. However, scope limitations follow physicians regardless of service delivery method.
What Continuing Education Must Family Physicians Complete?

Family physicians must complete 50 continuing medical education credits annually to maintain board certification. The American Board of Family Medicine requires 200 total credits over each five-year certification cycle.
Half of required credits must come from Category I activities approved by accredited medical education providers. Acceptable sponsors include the American Academy of Family Physicians, American Medical Association, and Accreditation Council for Continuing Medical Education.
State medical boards impose separate continuing education mandates for license renewal. Requirements range from 20 to 100 hours biennially depending on state regulations. California requires 50 hours every two years, while Illinois requires 150 hours every three years.
Specialized continuing education applies to specific practice areas. Physicians prescribing controlled substances must complete courses on substance use disorders and safe prescribing practices. Doctors treating geriatric patients in California need 20% of education focused on geriatrics and elderly care.
Board certification maintenance includes longitudinal assessment examinations. Physicians answer medical knowledge questions quarterly throughout the certification cycle covering topics from dermatology to internal medicine. Failure to complete assessments results in certification loss and potential hospital privilege revocation.
Audit processes verify continuing education compliance. State boards randomly audit physician renewals, requesting documentation of completed courses. Physicians unable to provide adequate proof face license suspension until deficiencies correct.
What Complex Medical Conditions Must Family Doctors Refer?
Family physicians cannot manage severe mental illness, advanced cancer, complicated cardiovascular disease, or conditions requiring subspecialty expertise. Training limitations prevent primary care doctors from treating bipolar disorder, schizophrenia, or treatment-resistant depression without psychiatric consultation.
Family physicians can manage straightforward cases of anxiety and depression with first-line medications and supportive counseling. However, patients requiring multiple medication trials, intensive psychotherapy, or electroconvulsive therapy need psychiatric care from psychiatry specialists.
Cancer diagnosis and treatment exceed family medicine training. Oncologists design chemotherapy protocols, radiation oncologists plan treatment, and surgical oncologists perform cancer operations. Family physicians coordinate care but cannot prescribe chemotherapy or manage treatment complications.
Advanced heart disease needs cardiologist management. Heart failure requiring specialized medications, complex arrhythmias, and valvular disease demand subspecialty evaluation. Neurological conditions like multiple sclerosis, Parkinson disease, and epilepsy require neurologist expertise.
Endocrine disorders beyond basic diabetes and thyroid disease need endocrinologist care. Respiratory conditions like chronic obstructive pulmonary disease with frequent exacerbations require pulmonologist management. Rheumatologic conditions like inflammatory arthritis, lupus, and vasculitis need rheumatologist evaluation for definitive diagnosis and treatment.
The referral threshold varies by physician training and experience. Recent residency graduates may refer more frequently than experienced physicians comfortable managing complex cases.
How Do State Laws Restrict Family Physician Practice?
State medical practice acts define legal boundaries for physician activities, creating significant variation across different states. Each state legislature enacts laws governing medical licensing, scope of practice, and prescribing authority for health professionals.
Prescribing regulations differ substantially between states. Some states allow family physicians to prescribe all medication classes while others restrict Schedule II controlled substances. Telemedicine prescribing laws vary, with certain states requiring in-person examinations before controlled substance prescriptions.
Interstate practice laws affect care delivery methods. Physicians must hold licenses in every state where patients receive care. Interstate compacts allow limited multi-state practice, but controlled substance prescribing still requires state-specific DEA registration.
Professional liability insurance requirements vary by state. Minimum coverage amounts range from $200,000 to $1 million per occurrence. Medical board rules supplement state law with detailed practice standards governing continuing education, professional conduct, recordkeeping, and patient care standards.
State regulations also govern collaboration with nursing professionals including nurse practitioners and physician assistants. Some states require physician supervision while others allow independent practice for advanced practice nurses.
What Insurance and Payment Rules Limit Family Doctors?
Insurance company policies restrict family physician services through prior authorization requirements, network limitations, and coverage exclusions. Payers define which procedures, tests, and treatments family doctors can provide without specialist referral.
Prior authorization delays or prevents certain medical services. Insurance companies require advance approval for expensive imaging studies, specialty medications, and elective procedures. The administrative burden of prior authorization consumes physician and staff time, reducing actual patient care hours.
Coverage policies determine reimbursable services. Medicare and Medicaid limit family physician payment for procedures commonly performed by specialists. Payers reduce reimbursement rates when primary care doctors bill for advanced services, discouraging procedure performance.
Quality metrics affect physician payment. Insurance companies withhold reimbursement when doctors fail to meet performance benchmarks for disease management including hypertension control, diabetes screening, and preventive health measures. Step therapy protocols force medication sequencing. Insurers require failure of cheaper medications before approving expensive alternatives.
What Ethical Standards Prohibit Certain Medical Practices?
Medical ethics codes forbid practices that compromise patient welfare, professional objectivity, or public trust. The American Medical Association Principles of Medical Ethics establish behavioral standards for all physicians across every medical specialty.
Dual relationships create ethical violations. Physicians cannot treat patients with whom they have romantic, business, or close personal relationships. Sexual relationships with current patients constitute grounds for immediate license revocation in every state.
Financial conflicts of interest require disclosure. Physicians cannot accept pharmaceutical company payments, device manufacturer kickbacks, or research funding without informing patients. The Physician Payments Sunshine Act mandates public reporting of industry payments exceeding $10 annually.
Patient autonomy rights prevent coercive practices. Physicians cannot force treatment on competent adults who refuse care. Informed consent requires explaining risks, benefits, and alternatives before procedures including physical examination findings and treatment options.
Confidentiality obligations protect patient privacy. Doctors cannot share medical information without permission except for treatment coordination, legal requirements, or public health reporting. HIPAA violations trigger federal fines up to $50,000 per violation.
Resource allocation decisions must follow justice principles. Physicians cannot deny care based on race, religion, sexual orientation, socioeconomic status, or ability to pay. Professional competence standards require staying within training boundaries and recognizing when specialist expertise exceeds generalist capabilities.
How Do Family Physicians Coordinate Specialty Care?
Family doctors serve as central coordinators who manage patient referrals, compile medical records, and integrate specialty recommendations into comprehensive care plans. This coordination role distinguishes primary care from specialist practice across all health care settings.
Medical home models center on family physician coordination. Patients receive all preventive services, chronic disease management, and acute care coordination through their primary doctor. Family physicians track specialist visits, review consultant recommendations, and adjust treatment plans accordingly.
Referral processes require detailed communication. Family doctors send clinical summaries, test results, and specific consultation questions to specialists in internal medicine, dermatology, and other subspecialties. After evaluation, specialists return recommendations that family physicians implement or modify based on patient circumstances.
Medication reconciliation prevents drug interactions and duplications. Family physicians maintain complete medication lists including specialist prescriptions, over-the-counter drugs, and supplements. Care transitions require family physician involvement to prevent medication errors and preventable complications.
Comprehensive practices like South Florida Med Group integrate primary care, mental health services, and specialized programs including weight management and ADHD treatment under one roof.
What Technology Restrictions Affect Modern Family Practice?
Federal and state telemedicine regulations limit remote prescribing, interstate practice, and virtual care delivery methods. Technology capabilities exceed current legal frameworks, creating practice restrictions for health professionals.
Controlled substance prescribing via telemedicine requires special DEA registration. The proposed special registration rule allows Schedule III-V prescribing for patients with access barriers. Schedule II medications need advanced telemedicine registration restricted to board-certified specialists treating vulnerable populations.
Electronic health record requirements mandate specific documentation standards. Meaningful use regulations dictate how doctors record patient encounters, prescribe medications, and share information electronically. Non-compliance results in Medicare payment penalties up to 5% of reimbursement.
Privacy regulations restrict technology use. HIPAA rules prohibit unsecured communication methods including regular email, text messaging, and non-encrypted video platforms. Artificial intelligence applications lack regulatory approval for independent medical decision-making. Physicians cannot rely solely on AI diagnostic tools or treatment algorithms.
Remote monitoring technology creates new liability exposures. Wearable devices and home monitoring systems generate continuous data streams that physicians must review and act upon. Failure to respond to abnormal readings can constitute negligence.
What Questions Should Patients Ask Family Doctors About Limitations?
Informed patients receive better health care by understanding physician capabilities and boundaries. Direct questions about training, experience, and referral decisions improve treatment outcomes.
Patients should ask whether family doctors can manage specific conditions. Some problems require immediate specialist referral while others fall within primary care scope. Prescribing authority questions prevent medication errors. Patients should verify whether family doctors can prescribe needed medications or require specialist involvement.
Care coordination questions identify communication plans. Patients should understand how family doctors share information with specialists, review test results, and integrate recommendations into treatment plans.
Emergency coverage questions reveal after-hours access. Patients need clear instructions for urgent problems, weekend concerns, and situations requiring immediate specialist attention from emergency medicine providers. Insurance coverage questions prevent surprise bills by confirming whether proposed treatments require prior authorization or specialist referral for coverage.
Final Thoughts
Family practice physicians face numerous legal, ethical, and practical limitations that protect patient safety and promote quality care. Doctors cannot treat immediate family members, prescribe without proper authorization, perform major surgery, or manage conditions outside their training.
State medical practice acts, federal regulations, insurance policies, and professional ethics codes create overlapping restriction systems. These boundaries vary by location, practice setting, and individual physician qualifications. Understanding limitations helps patients navigate the health care system effectively.
Restrictions benefit patients by directing them to appropriately trained health professionals. Family doctors recognize their boundaries and refer complex cases to subspecialists in fields like psychiatry, internal medicine, dermatology, and geriatrics. This collaborative approach produces better outcomes than attempting care beyond training limits.
Family physicians provide comprehensive services within their scope. Preventive care, chronic disease management including hypertension and diabetes control, acute illness treatment, and care coordination remain core family medicine functions. The breadth of residency training and continuing medical education enables doctors to address most health concerns patients encounter.
South Florida Med Group provides comprehensive services within appropriate practice boundaries. The medical team combines primary care, mental health treatment, and IV infusion therapy while referring patients needing specialized care. Services address common conditions including bipolar disorder, PTSD, and chronic medical problems requiring ongoing management.
Schedule your appointment to receive coordinated care from experienced family medicine providers who understand professional limitations and practice within appropriate boundaries.
.png)
.png)
.png)



.png)
.png)
.png)

.png)

.png)